We saw Dr P yesterday morning, and the news was mixed. The PSA at the last test was 47 — a rather unenviable record — even a PB. There are always “howevers”, though, and here they are:
- Dr P said he would need three consecutive rises in the PSA to consider changing my treatment (i.e. to chemotherapy).
- In any case, he can’t move on this while I am having the radiation treatments at Peter Mac. Fortunately
- He thinks there is no urgency to go with some more chemo.
- I should be finished at Peter Mac by mid-September. This fits in with my next appointment with Dr P. So there should be no WICOS problem. (This is a useful acronym for “Who’s In Charge of The Ship”.)
- By mid-September, I will also have had my regular three-monthly CT head and neck and bone scan. From this, Dr P will have hard evidence on whether to embark on another round of chemo.
- Dr P said “On paper, you look terrible, but in person, you look fantastic”. (You will all remember that he places more store in the latter than the former.)
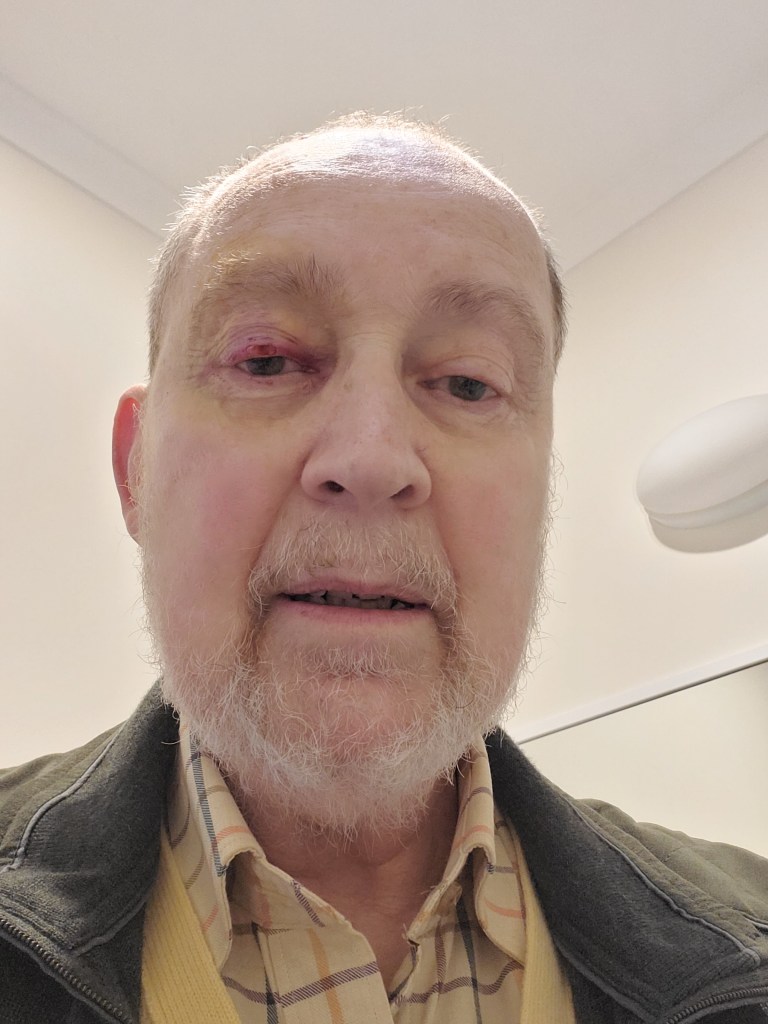
I certainly feel fine, and haven’t noticed too many side effects from the radiation treatment. What side effects I have noticed are a bit more fatigue, and a slight loss of focus in my left eye (the one being irradiated). I have reported the latter to my radiation oncologist; the effect should be temporary. I still have enough focus in the left eye to drive; I guess also the right eye takes over somewhat to compensate. (I have to stress that the radiation therapists take great care to shield those areas of the eye not being irradiated. Doing this takes most of the appointment — the actual radiation only takes a few minutes.)
Today I start the double appointments, i.e. the left eye first, then the head and neck area. Because they are done on different machines, they have to be separate appointments. But the Peter Mac folk have brought them as close together as possible. Getting in and out to these appointments should be easier from next week, when patient transport via the ambulance service will start. (I blogged about this in One Week In .) I found, after about an hour of fooling around on the Ambulance Victoria site, your doctor has to get the ball rolling on this. Fortunately, before I embarked on the DIY approach, I had first left a phone message with the Peter Mac patient transport folk. They rang me back, and it was all set up.
Meanwhile I have two more days remaining of being driven in by my beloved. I am not only deeply appreciative of her doing this, but I also get to chat with her at a time when she would normally be working, which is really lovely. She has also stepped up to the plate, as it were, in the kitchen. Truly a heroine!
Season 3 of Only Murders In The Building is providing a good distraction from all this. Disney+ is doling these out somewhat; as of 8 August, only two episodes had dropped, which we watched one after the other. Apparently this belongs to the genre, probably invented by Agatha Christie, known as “Cosy Murder”. For those who would like to check this show out, APPARENTLY OnePass offers a free 14 day trial of Disney+. (The all caps denote that I haven’t tried this offer myself. No care or responsibility taken. Unfortunately I’m not getting paid anything for this promotion.) I think Seasons 1 & 2 are still available. As Peter Cundall used to say — OK, that’s your bleeding lot!